Ravi didn’t know it, but he, like millions of Americans, was trapped in a “ghost network.” As some of those people have discovered, the providers listed in an insurer’s network have either retired or died. Many other providers have stopped accepting insurance — often because the companies made it excessively difficult for them to do so. Some just aren’t taking new patients. Insurers are often slow to remove them from directories, if they do so at all. It adds up to a bait and switch by insurance companies that leads customers to believe there are more options for care than actually exist.
Ambetter’s parent company, Centene, has been accused numerous times of presiding over ghost networks. One of the 25 largest corporations in America, Centene brings in more revenue than Disney, FedEx or PepsiCo, but it is less known because its hundreds of subsidiaries use different names. In addition to insuring the largest number of marketplace customers, it’s the biggest player in Medicaid managed care and a giant in Medicare Advantage, insurance for seniors that’s offered by private companies instead of the federal government.
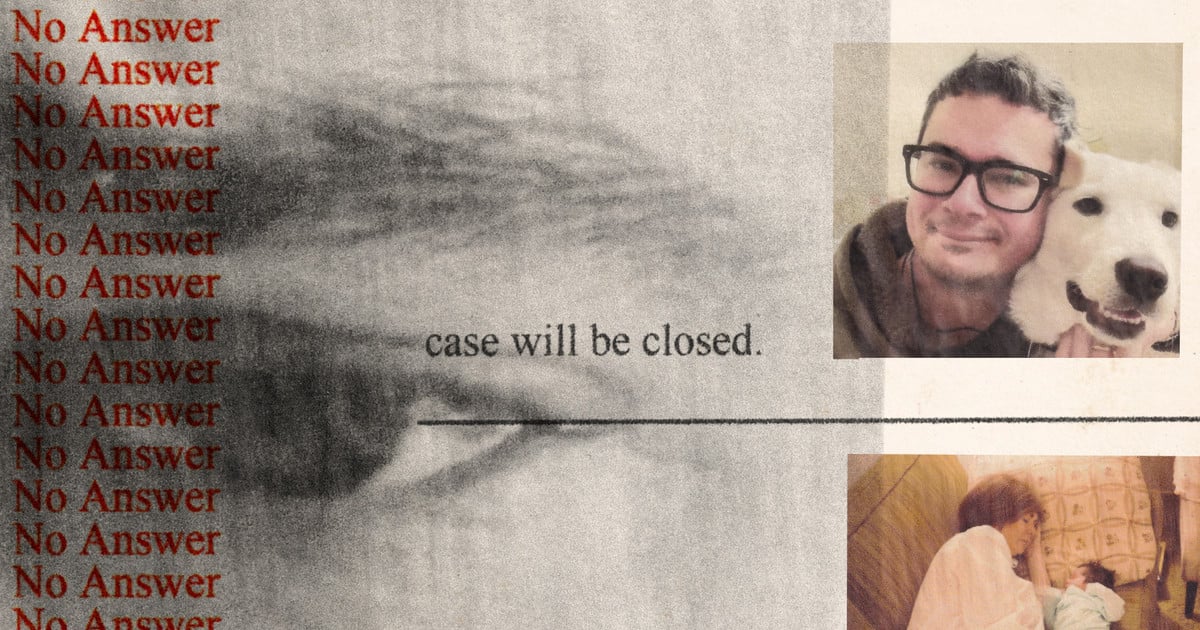
ProPublica reached out to Centene and the subsidiary that oversaw Ravi’s plan more than two dozen times and sent them both a detailed list of questions. None of their media representatives responded.


Health Net is one of Centene’s companies and they pull this crap and worse every single day.
Health Net’s provider lists includes a huge number of ghost providers. In my case even the ones that were real were the wrong kind of specialists. Heath Net insisted I go to these providers despite the fact they couldn’t help me and refused to see me.
I ended up having to regularly make a 220 mile trip to get the healthcare I needed.
It gets worse. Health Net regularly refused payment for services that were covered under their policy. I easily spent 10 hours a week on the phone trying to get legitimate claims paid by this horrible company. The first 45 minutes of the calls were spent trying to get past their first line “customer service” people to someone who could actually deal with the problem. Health Net repeatedly refused coverage on DME that they had previously paid for and said the previous approvals were a mistake. They weren’t.
Health Net even refused payment for a visit to specialist after they had provided pre-approval for the visit in writing. It took seven months and probably 20 hours on the phone before the crooks paid the bill.
Centene and their subsidiaries should be shut down and their executives should be in prison.